"Cheap 100 mg januvia fast delivery, managing diabetes in dogs".
By: F. Ramirez, M.B. B.CH. B.A.O., Ph.D.
Vice Chair, Charles R. Drew University of Medicine and Science College of Medicine
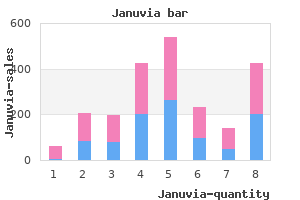
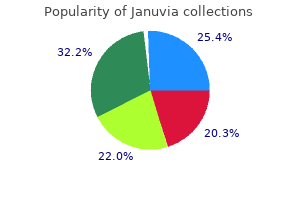
Then foam rubber forms were manufactured with holes in the back for metal weights to add stability and gravity diabetes symptoms of foot neuropathy purchase januvia 100 mg amex. It is very rare diabetes epidemic buy januvia online pills, but possible, to require custom manufacturing of the form for irregular mastectomy defects. The external prosthesis is completely concealed in a bra with an adjustable built-in pocket specially constructed to accommodate it. Wearing the weighted prosthesis should help the body maintain its posture and balance and may prevent back and neck strain. With the concern that the prosthesis could become dislodged, even with such a specially fitted bra or swimsuit, adherent forms have now become popular. Using a variety of surgical adhesives, the form adheres to the chest wall or to a backing on the skin of the chest wall, so that the form can be removed every night while the backing can remain for a week or more. In retrospective studies, 1,2 the differences among those opting for breast reconstruction, those wearing external prostheses, and those doing neither were explored. Today, the survivor-to-patient outreach and support include volunteers who have had breast conservation and postmastectomy reconstruction. Resources for the patient include breast prostheses information with knowledge of local resources, clothing suggestions, and even an exercise booklet and aids. The traditional concept of performing the mastectomy, proceeding with adjuvant therapy, and delaying reconstruction until the completion of adjuvant therapy is being supplanted by the increasing use of immediate reconstruction. In a mastectomy without immediate reconstruction, it is difficult to "save" any extra native breast skin because, with the volume of the breast missing, there is excess skin folding and wrinkling. The first large report of immediate reconstruction was in 1982 by Georgiade et al. Because the mastectomy and reconstruction are performed under a single anesthetic, the total hospital costs and convalescent time are reduced when compared to mastectomy and delayed reconstruction. Current methods of reconstruction can be broadly classified into autologous tissue or prosthetic material. Prosthetic reconstruction uses a process known as tissue expansion to create a "pocket" for the ultimate placement of a breast implant. There are occasional indications for a combination of both autologous tissue and an implant. The selection of the reconstructive technique is based on anatomic patient factors, including the laxity and thickness of the remaining chest wall skin, the condition of the chest wall musculature, the size of the opposite breast, and the availability of suitable autologous tissue donor sites. Initially, implants were placed directly under the skin in the mastectomy space, but the results were limited by the available skin envelope and capsular contracture. Current techniques use a complete submuscular placement of the tissue expander, with coverage by pectoralis major, serratus anterior, and occasionally the anterior rectus sheath. The area is allowed to heal for approximately 10 to 14 days, at which time fluid expansion is commenced. Using an integrated valve within the expander, saline is injected into the expander percutaneously until the appropriate size is reached (. The exchange to a permanent breast implant takes place after the chemotherapy course. Using a two-stage method of implant reconstruction allows for maximum control of the implant pocket and optimal symmetry with the contralateral breast (. When indicated, contralateral symmetry procedures such as augmentation mammoplasty, reduction mammoplasty, or mastopexy (breast lift), are accomplished when the tissue expander is exchanged to a permanent implant. Complete submuscular placement of the tissue expander at the time of mastectomy (left). Percutaneous approach to expansion using a complete submuscular integrated valve tissue expander (right). A: After expansion is complete, the pocket is overexpanded relative to the normal breast to maximize ptosis and implant projection. B: the same patient subsequent to exchange of the tissue expander to a permanent saline breast implant followed by nipple-areola reconstruction and tattooing. In this series, premature removal of the tissue expander secondary to wound-related complications or persistent disease was necessary in only 1.
If the pregnancy is in the first trimester blood glucose a1c conversion discount januvia 100mg with mastercard, external-beam irradiation can be started with the expectation that spontaneous abortion will occur before the delivery of 40 Gy blood sugar danger zone buy januvia canada. In the second trimester, a delay of therapy may be entertained to improve the chances of fetal survival. If the patient wishes to delay therapy, it is important to ensure fetal pulmonary maturity before delivery is undertaken. Compared with other cervical cancer patients, those with cervical cancer during pregnancy have slightly better overall survival because an increased proportion have stage I disease. The diagnosis of cancer in the postpartum period tends to be associated with a more advanced clinical stage and a corresponding decrease in survival. However, studies differ in their conclusions about whether pregnancy has an independent influence on the prognosis of patients with cervical cancer. At least 13 cases demonstrating this unusual pattern of failure have been reported. For this reason, in patients with an intact uterus, it is probable that many tumors that originated in the apical vagina are actually classified as cervical cancers. This may explain why a large percentage (30% to 50%) of patients diagnosed with vaginal carcinoma have had a prior hysterectomy (preventing classification of their tumors as primary cervical cancers). Pride and colleagues 505 suggested that pelvic irradiation might be a predisposing factor in some cases. However, viral and other risk factors independent of the mode of treatment undoubtedly place some of these patients at risk for multiple primary tumors. In a review of 301 patients with vaginal cancer, Chyle and associates 495 found that 56 had a prior history of carcinoma in situ of the cervix, 22 had a history of invasive cervical cancer, and two had prior in situ carcinomas of the vagina. Primary invasive carcinoma of the vagina is predominantly a disease of elderly women, with 70% to 80% of cases presenting in women older than 60 years. This led to the establishment of a registry to gather information about cases of clear cell carcinoma in the United States. The oldest patient reported so far was 42 years old at diagnosis, but the risk to women older than 40 years is still unknown because women in the first exposed cohort are just reaching their fifth decade. Tumors may invade directly to involve adjacent structures such as the urethra, bladder, and rectum. Vaginal cancers may also spread laterally to the paravaginal space and pelvic wall. The vagina is supplied with a fine anastomosing network of lymphatics in the mucosa and submucosa. Despite the continuity of lymphatic vessels within the vagina, Plentl and Friedman 515 found a regular pattern of regional drainage from specific regions of the vagina. The lymphatics of the vaginal vault communicate with those of the lower cervix, draining laterally to the obturator and hypogastric nodes. The lymphatics of the posterior wall anastomose with those of the anterior rectal wall, draining to the superior and inferior gluteal nodes. The lymphatics of the lower third of the vagina communicate with those of the vulva and drain either to the pelvic nodes or with the vulvar lymphatics to the inguinofemoral lymph nodes. Plentl and Friedman summarized their description of the lymphatic drainage of the vagina with the comment that, except for the lateral external iliac group, all lymph nodes of the pelvis may at one time or other serve as primary sites of regional drainage for vaginal lymph. In a review of early reports, Plentl and Friedman 515 quoted an overall incidence of positive nodes of 21%. Approximately one-third of these tumors are keratinizing, and more than one-half are nonkeratinizing, moderately differentiated lesions. Verrucous carcinoma is an uncommon variant of squamous cell carcinoma that presents as a warty, fungating mass. This tumor rarely metastasizes but can extensively infiltrate into surrounding tissues, including the rectum and coccyx. The differential diagnosis of adenocarcinoma occurring in the vagina is often difficult, as it must be distinguished from metastatic tumors originating in other sites. It has been hypothesized that these tumors may arise in foci of adenosis, from mesonephric rests, or from foci of endometriosis in the vagina.
Buy januvia with visa. Ketones and Diabetic Ketoacidosis | Knowing the Signs and Symptoms.
The double-staple technique of Knight and Griffin is most commonly used to restore intestinal continuity after resections in which a short rectal stump remains (Griffin diabetes medications that start with g order januvia with amex, 1990) diabetes que es generic januvia 100mg line. Mucosal Margins Attaining tumor-free margins at the edges of a rectal cancer resection specimen is the hallmark of curative surgical therapy. The purpose of obtaining such a margin is to prevent local failure and effect cure. Spread beyond the lower edge of a rectal cancer may occur by submucosal spread in intramural lymphatics. Fewer than 5% of rectal cancers show distal mucosal spread beyond the edge of the tumor, and only 2. Margins may need to be increased in locally aggressive tumors, such as those showing poor differentiation or vascular and lymphatic invasion. It does not appear that a mural mucosal margin of 5 cm is necessary to prevent local recurrence. Even margins of 1 cm have been demonstrated to provide adequate protection from local recurrence in the absence of aggressive histologic features. However, some have proposed that distal margins may be reduced in the face of preoperative chemoradiation. These concepts have allowed for an increase in sphincter-preserving procedures without detracting from local control and survival. Many patients have residual microscopic disease within the bowel wall, despite a complete response at the mucosal surface. The difference between margins reported in the literature and margins in situ at surgery can be significant. This fact is due to contraction of the specimen after its excision and the stretching of the rectal wall. A microscopically involved margin is unacceptable for a curative resection and will not be salvaged by radiation and chemotherapy. The need for negative mural margins also applies to local excision specimens for which a 1-cm margin of grossly normal bowel wall around the tumor is recommended for satisfactory resection. The proximal extent of the mesorectum and the rectosigmoid mesentery should be included in the resection. Lymph node excision at the base of the inferior mesenteric artery does not enhance survival compared with lymph node excision just distal to the origin of the left colon. This is particularly true for low rectal cancers in which positive nodes between the left colic origin and the inferior mesenteric artery origin are found in fewer than 6% of resectable cases. Retroperitoneal adenopathy above the level of the inferior mesenteric artery is frequently a harbinger of occult systemic spread that is not amenable to cure by surgery alone. Total Mesorectal Excision the mesentery of the rectum contains its blood supply and lymphatics in a bilobed fat packet situated immediately posterior and lateral to the thick-walled rectum. The majority of resectable primary rectal tumors and involved lymph nodes in rectal cancer specimens are found within this structure. Because the mesorectum tapers as it proceeds distally, it is totally excised for most middle and lower rectal cancers. More proximal rectal tumors can be treated by a mesorectal excision extending 5 cm beyond the lower tumor edge. Total mesorectal excision has been associated with a high rate of anastomotic leak when used for upper rectal tumors. The work of Quirke and others (1986) has dramatically demonstrated the importance of lateral tumor spread in the local recurrence of resected rectal cancers (Table 33. Among patients with local recurrence, tumor involvement at the circumferential margin of resection has been found in 85% of cases. Because of difficulty in obtaining adequate exposure in the low pelvis and the surrounding structures, circumferential margins around rectal cancer can be highly variable and minimal. Surgical experience and surgical technique have demonstrated their key role in the prevention of local recurrence by controlled sharp dissection done with attention to these margins. Up to 23% of patients can have mesorectal tumor implants aside from discrete nodes. Distal Mesorectal Spread in Producing an Involved Radial Margin Circumferential clearance of rectal tumors by total mesorectal excision has become the accepted surgical procedure for the management of most rectal cancer. Total mesorectal excision by full mobilization of the rectum along anatomic planes has been demonstrated to be effective in the surgical management of rectal cancer. Lateral Pelvic Lymph Node Dissection Lymphatic drainage of the rectum not only flows proximally along the inferior mesenteric vessels, but also follows the middle rectal vessels to the lateral pelvic sidewall and into internal iliac nodes.
In a regional lymphadenectomy blood glucose diabetes buy januvia amex, ipsilateral nodal tissue from the diaphragm to the bifurcation of the aorta as well as nodal tissue in the interaortocaval region at the hilum of the kidney is removed treatment diabetes uk cheap januvia 100 mg with mastercard. Proponents of regional lymphadenectomy point out that 5-year survival in patients with node-positive renal carcinoma is greatly decreased, and there is no known effective therapy for metastatic renal carcinoma. If local nodes were the first site of metastasis, resection of microscopic disease might be of benefit. Long-term survival in patients with node-positive disease who underwent lymphadenectomy has been reported. In patients in whom all visible disease has been resected surgically, most physicians recommend treatment when residual or recurrent disease becomes detectable. Bilateral Renal Carcinoma or Tumors in Solitary Kidneys the treatment of patients with either bilateral renal carcinoma or renal carcinoma in a solitary kidney is challenging. Patients with tumor in a solitary kidney may be treated by either partial nephrectomy or nephrectomy followed by dialysis or transplantation (or both). This ex vivo procedure entails radical excision of the kidney and division of the ureter. The kidney then is placed on a table and is intermittently perfused with a chilled solution to enhance viability. Under optical magnification, the tumor is carefully dissected from the surrounding renal parenchyma. Care is taken to preserve the vasculature of the normal kidney, which has been defined by preoperative arteriography. A small rim of normal tissue is removed along with the tumor to provide a tumor-free margin of resection. After the kidney has been surgically reconstructed, it is autotransplanted back into the iliac space. Vascular anastomosis of the renal artery and vein to the iliac vessels and ureteroureterostomy are performed. Surgical Management of Patients with Hereditary Forms of Renal Carcinoma Patients with hereditary forms of renal carcinoma are often challenging to manage. Previous reports have demonstrated increased complication rates using conventional radiotherapeutic techniques. However, recent studies have suggested that the use of more sophisticated radiation techniques is less likely to result in treatment-related complications. Though some retrospective reports have indicated an improvement in local tumor control or overall survival with the addition of postoperative radiotherapy, 95,101,102 subsequent randomized prospective trials could not confirm any benefit. In fact, a trend for an inferior 5-year survival outcome was observed for the adjuvant radiotherapy group (36% as compared to 47% for patients with nephrectomy), owing to a higher complication rate observed in these patients. Ten years later, a second randomized prospective trial comparing nephrectomy and postoperative radiotherapy to nephrectomy alone demonstrated identical results. Further, the incidence of treatment-related morbidity in these two randomized trials was unacceptably high. Severe complications were experienced in 20% to 44% of treated patients, with an associated increased mortality rate due to radiation-related toxicities. The potential value of preoperative radiotherapy has also been tested in two randomized trials,97,98 neither of which could demonstrate any advantage for improved local control or survival with adjuvant radiotherapy. Previously published postoperative studies used relatively crude radiation techniques, and the radiation dose per fraction of 250 cGy to cumulative doses of 5000 to 5500 cGy used in some reports likely directly contributed to the high gastrointestinal and liver-related toxicities observed. In addition, a significant percentage of patients treated in these trials did not have prognostic features indicating a high risk for local recurrence for which adjuvant radiotherapy may have been potentially beneficial. Based on patterns-of-failure studies after nephrectomy alone, 103,104 the overall local recurrence rate is low, and routine administration of adjuvant local therapy for all patients on the basis of advanced stage only would not be expected to improve outcome. However, among patients with positive surgical margins or positive lymph nodes, the incidence of local recurrence was 21%. Advanced T-stage disease in the absence of these prognostic features did not predict for local recurrence and thus is not necessarily an indication for local adjuvant therapy. More recent reports have demonstrated that with the application of more sophisticated radiotherapeutic planning techniques, the incidence of treatment-related complications has been minimal.