"Buy generic accutane 30mg on line, acne before period".
By: M. Wenzel, M.A., M.D.
Vice Chair, The Ohio State University College of Medicine
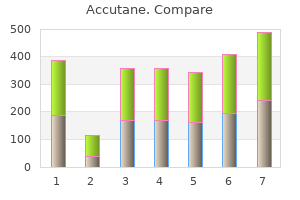
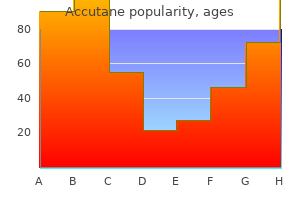
It would be more effective skin care questionnaire template 5mg accutane for sale, therefore acne moisturizer buy accutane 10 mg line, to implement general screening at the age of 4 weeks. The problem with this approach is that not all infants can be reliably tracked down at this age, whereas they are already in the maternity ward at birth and have to undergo a comprehensive examination in any case. The ultrasound scan is possible up until the time of ossification of the femoral head center, generally up to the age of 9, or a maximum of 12, months. If general screening is not available, the ultrasound examination should at least be indicated if certain broadly interpreted risk factors are present. The corresponding risk factors are: a family history of hip dysplasia or coxarthrosis, premature birth, breech presentation, other skeletal anomalies, oligohydramnios, clinical suspicion of hip dysplasia. These indications have become generally accepted throughout the German-speaking world, whereas ultrasound scanning is much less widespread in Englishspeaking countries. On the other hand, the incidence of hip dysplasia is also much lower in these countries, where the ultrasound method is only used in a few centers if risk factors are present. If the costs of sonographic screening are taken into account, the overall costs are no higher than with purely clinical screening. There is still some dispute, however, as to whether the ultrasound examination should be performed only if risk factors are present or on a universal basis [46, 64]. The above mentioned Dutch study also showed that a very small proportion of initially normal hips became abnormal at 3 months (0. To sum up: ultrasound examination is a valuable addition to the diagnostic arsenal for investigating the hip in infants. Hip dysplasias can be detected at an early stage with a considerable degree of certainty with the Graf method. Universal screening is essential in Central Europe in view of the relatively high incidence of hip dysplasia in these countries. If screening is not possible, sonographic examination is indicated in the presence of certain, broadly interpreted risk factors. If applied meticulously, the Graf technique provides a highly reliable overall picture, even if the correspondence in respect of individual parameters viewed in isolation is not particularly good. Treatment As ultrasound becomes more widespread, concerns are often expressed, particularly by health insurers, about the growing trend of the administration of unnecessary treatments. Abduction splinting should not be prescribed simply because of uncertainty about the interpretation of the ultrasound findings since it can also have side effects (femoral head necrosis). Conservative treatment the following types of treatment are differentiated: maturation treatment, closed reduction, immobilization. These are made of a plastic material and incorporate a rigid bar placed between the legs. High rates of avascular necrosis were reported during the first few years of abduction splinting [83], at a time when these orthoses were used for reductions. This produces less pronounced abduction but greater flexion than standard abduction pants. Since it is made from plastic, hygiene is less of a problem than with the Pavlik harness, for example, which is made of fabric. Reduction methods Manual reduction methods are of historical significance only as the associated complication rates were far too high. Reduction braces We differentiate between the following options: manual reduction methods, braces for reduction, traction methods. The Pavlik harness [65] incorporates two shoulder straps that cross over at the back and are fastened to a broad chest strap which fastens at the front (. The lower legs are enclosed by stirrup-like straps, with the topmost strap encircling the leg just below the knee. The distance between the chest strap and the lower legs can be adjusted separately by means of buckles at the front and back. This repositioning of the dislocated hip can take a few days in some children, but may require several weeks in others.
Diagnosis is based on the visualization of an abnormal appendix or pericecal inflammation or abscess with or without the presence of an appendicolith skin care 9 discount accutane. This type of imaging can supplement or supplant abdominal ultrasound studies; plain abdominal films are of limited value skin care shiseido effective accutane 10 mg. How specific is the diagnosis of appendicitis if an appendicolith is noted on radiograph? The positive-predictive value of finding an appendicolith is about 75%; in its absence, the negative-predictive value is only 26%. Should a digital rectal examination be performed on all children with possible appendicitis? Tradition says yes, but reviews of studies of the practice indicate that in children it can be emotionally and physically traumatic and associated with a high false-positive interpretation. It may be most helpful in equivocal cases involving pelvic or retrocecal appendicitis (about one third of cases), suspected abscess formation, or for attempted palpation of adnexal or cervical tissues when vaginal examination is not indicated. Thus, many clinicians now view it as "investigatory" rather than "routine" and only when results will change management. In children taken to surgery for suspected appendicitis, how often is perforation of the appendix present? It depends to a large extent on the age of the child (and, of course, on the skill of the clinician). Unfortunately, as a result of the variable location of the appendix, the clinical presentation of pain in appendicitis is often very different from the classic case. In infants younger than 1 year, nearly 100% of patients who come to surgery have a perforation. Fortunately, appendicitis is rare in this age group because the appendiceal opening at the cecum is much larger than the tip, and obstruction is unusual. In children younger than 2 years, 70% to 80% are perforated; in those 5 years and younger, 50% are perforated. Particularly in younger children, a high index of suspicion is necessary, and rapid diagnosis is critical. If the onset of symptoms can be pinpointed (usually anorexia related to a meal), 10% of patients will have perforation during the first 24 hours, but more than 50% will perforate by 48 hours. A controversial question because a long-held fear has been that treating the pain may mask the symptoms, change the physical findings, and potentially delay the diagnosis of a possible surgical problem. However, there is a growing evidence that the use of opiate analgesia in patients, including children, with acute abdominal pain does not result in increased mortality or morbidity. Bailey B, Bergeron S, Gravel J, et al: Efficacy and impact of intravenous morphine before surgical consultation in children with right lower quadrant pain suggestive of appendicitis: a randomized controlled trial, J Pediatr 50:371378, 2007. What genetically inherited disease has the highest known mutation rate per gamete per generation? The clinical features are cafe-au-lait spots and axillary freckling in childhood followed by the development of neurofibromas in later years. There is about a 10% risk for malignancy with this condition, and mental deficiency is common. Which disorders with ethnic and racial predilections most commonly warrant maternal screening for carrier status? Why are mitochondrial disorders transmitted from generation to generation by the mother and not the father? Transmission to males or females is equally likely; however, expression is variable because mosaicism with normal and abnormal mitochondria in varying proportions is very common. Advanced paternal age is well documented to be associated with new dominant mutations. The assumption is that the increased mutation rate is the result of the accumulation of new mutations from many cell divisions. The mutation rate in fathers who are older than 50 years is five times higher than the mutation rate in fathers who are younger than 20 years.
Discount accutane 10 mg with amex. CHANEL SUBLIMAGE: how to intensely revitalize your skin.
If possible acne garret buy accutane 40 mg fast delivery, this consultation process acne at 40 cheap accutane online american express, including a discussion of the radiographic findings, should clarify the following questions: 593 4. The history, clinical and radiological findings provide an indication of the type of lesion involved (tumor, tumor-like lesion, inflammation, metabolic bone changes or a (post-) traumatic situation). The differential diagnostic ranking will produce various options for substantiating or ruling out clinical conditions by means of additional investigations. An undifferentiated sarcoma, for example, can be identified as an osteosarcoma if enzyme histochemical tests are positive for alkaline phosphatase. The same applies to molecular biological investigations and the detection of the translocation that is typical of Ewing sarcoma. Can the additional investigations and/or likely required therapeutic procedures be implemented on site? If the doctor lacks the diagnostic and therapeutic experience, irreparable mistakes that impair the prognosis can be made even at the biopsy stage. Consequently, the decision as to whether the patient can subsequently be treated on site or will need to be transferred to a specialist hospital must be made before the biopsy. Remarks on the biopsy procedure of the biopsy material should be examined histologically (unless it is required for any other special investigations), otherwise there is a risk that diagnostically crucial findings, which are often only present in small sections in bone tumors with a heterogeneous structure, may be overlooked. In addition to matrix formation (osteoid, chondro-osteoid, hyaline cartilaginous or myxoid cartilage matrix), the cellular composition of the lesion in particular should be examined, and the pathologist will need to establish, whether any matrix is formed from tumor cells or whether. It should always be borne in mind that giant cells occur in numerous lesions and can frequently confuse the diagnostician. Pseudocystic, blood-filled cavities are also not necessarily synonymous with the diagnosis of an aneurysmal bone cyst, but can also occur as secondary phenomena as constituents of other lesions. The possibility of callus-like new bone formation with superimposed microfractures should also be considered. For these reasons, the tentative histological diagnosis should always be checked against the conventional x-ray. If any discrepancies arise between the radiological and the histological diagnosis, and if these are not satisfactorily resolved in the interdisciplinary discussion, even including one with experienced specialists, a further biopsy should be performed, possibly in a center with corresponding diagnostic and therapeutic experience. If the differential diagnostic alternatives are clear and the patient can be treated on site, the orthopaedist and pathologist must agree on the timing of the biopsy. If it is not macroscopically obvious, the peripheral end of the tumor should be marked (suture, ink). The pathologist must possess precise knowledge, on the basis of the x-ray, of the biopsy site. The tissue should be well cooled (but not frozen) as soon as possible (ideally under frozen section conditions) and forwarded for further investigations. Imprint cytology can be used to prepare unfixed biopsy material and samples shock-frozen for additional investigations (see above). A frozen section diagnosis is then required only if it involves therapeutic consequences. The frozen section evaluation can be helpful in ensuring that representative tumor tissue has been collected so that further material can be biopsied in the same session if necessary. For these reasons Enneking [2] has introduced a separate staging system for bone tumors that takes account of the following parameters: the histological differentiation grade (G), the anatomical situation of the tumor (T). In respect of the histological differentiation grade (G), G0 refers to a benign tumor, G1 to a highly differentiated (lowgrade) malignant tumor, and G2 to a poorly differentiated, high-grade malignant tumor. As regards the anatomical situation (Site: T) we distinguish between T1, intracompartmental tumors, and T2, extracompartmental tumors. Metastases are either not detectable (M0) or have been confirmed by imaging investigations (M1). Staging of the tumor enables the orthopaedist to decide on the appropriate treatment (Chapter 4. Apart from the histological differentiation grade (G), the anatomical situation of the tumor (T) i. Part of the correct biopsy procedure includes the appropriate planning of the potential access route as this must also be taken into consideration at the time of resection. Many mistakes are also made in relation to benign tumors and tumor-like lesions. Malignant tumors should always be treated in a specialist center with a multidisciplinary team (including, in addition to an orthopaedist specialized in tumors, an oncologist, a pathologist with experience in sarcoma diagnosis, a musculoskeletal radiologist and a radio-oncologist) [7].
Therefore skin care acne buy cheap accutane 20mg on-line, a high index of suspicion with a low threshold for surgical exploration is required to ensure these injuries are not missed skin care lines for estheticians discount 20 mg accutane. Tendon repair is not an emergency; however, as time progresses the repair becomes more difficult as the cut ends retract, tissue becomes more oedematous and scarred, and the prognosis worsens. A delay of 1014 days will require secondary repair owing to tendon swelling, tendon contraction and muscle fibrosis (Griffin et al. Tendons should be handled with care during surgery because excessive manipulation causes trauma and leads to scarring and adhesion formation. The first technique used for flexor tendon repair was described in 1917 (Kleinert et al. Since then, several surgical approaches have been suggested; these implement contradictory ideas about optimal management. The strength of a tendon repair is affected by a number of factors, primarily (Griffin et al. The simplest repair technique is a two-strand approach such as the Kessler technique (Figure 7. Increasing the number of sutures crossing the repair site has been shown to improve the strength of repair. However, a greater number of strands requires more handling of the tendon, increasing the risk of trauma and subsequent scarring. It is also technically more demanding and inappropriate placement of sutures can lead to a load imbalance on the tendon (Winters et al. The ideal suture material for flexor tendon should provide adequate tensile strength for long enough to allow the tendon to heal. Non-absorbable synthetic sutures such as monofilament nylon, braided polyester and monofilament polypropylene have A B C D E figure 7. A number of synthetic tendon devices have been invented with the aim of improving post-operative outcome. Mersilene mesh sleeves, Dacron splints and internal stainless steel anchors have been tried but all were found to be unsuitable for clinical use. To date, there is not enough supporting experimental evidence to warrant the use of any such devices, but research into this field continues (Griffin et al. Rehabilitation after tendon repair is a balancing act between achieving functional movement and avoiding tendon rupture. Early mobilisation of tendons has been shown to produce stronger repairs with fewer adhesions (Tang, 2007); however, this may lead to an increased risk of tendon rupture. Patients may not regain full use of their hand for up to 3 months and may have to be off work for this period (Nakhdjevani and Ahmadi, 2007). Complications Complications following flexor tendon repair can be divided into early and late: Early complications infection, pain, tendon rupture, pulley rupture and poor tendon gliding. Late complications adhesions, stiffness, scarring and complex regional pain syndrome. Causes of rupture following surgery include tendon overload, oedema, misuse of the hand and early mobilisation (Griffin et al. Adhesions occur in approximately 20% of cases (Manske, 1988), causing stiffness and pain. They are treated with tenolysis, which can be performed 36 months after the initial tendon repair (Strickland, 1985). The only treatment for bowstringing is surgical pulley reconstruction (Mehta and Phillips, 2005). Tendon grafting Secondary tendon repair consists of removing the diseased or non-functioning tendon and grafting the defect with an autograft or allograft. Traditional autologous grafts include the palmaris longus, extensor digitorum longus and plantaris tendons. S of t t iS Su e i nj u rieS of t he hand 173 Single-stage grafting of the flexor tendon involves excision of the damaged tendon and its immediate replacement with the harvested tendon graft. However, this technique is usually not successful if the flexor sheath and pulley systems are disrupted.