"Generic 40/60mg cialis with dapoxetine otc, erectile dysfunction pump nhs".
By: T. Murat, M.A., M.D., Ph.D.
Co-Director, University of Washington School of Medicine
Furthermore erectile dysfunction treatment natural remedies effective 40/60 mg cialis with dapoxetine, readmission for any reason exposes the patient to risks associated with hospitalization impotence spell trusted cialis with dapoxetine 40/60mg, such as iatrogenic errors. Second, there is no reliable way to determine whether a readmission is related to the previous hospitalization based on the documented cause of readmission. For example, a stroke patient who develops aspiration pneumonia may ultimately be readmitted for respiratory distress. It would be inappropriate to treat this readmission as unrelated to the care the patient received for stroke. Third, the range of potentially avoidable readmissions also includes those not directly related to the index condition category, such as those resulting from medication reconciliation errors, poor communication at discharge, or inadequate follow-up post-discharge. Fifth, research shows that readmission reduction interventions can reduce all-cause readmission, not only condition-specific readmission. Finally, defining the outcome as all-cause readmissions may encourage hospitals to implement broader initiatives aimed at improving the overall care within the hospital and transitions from the hospital setting instead of limiting the focus to a narrow set of conditionspecific approaches. The goal of this measure is not to reduce readmissions to zero, but to assess hospital performance relative to what is expected given the performance of other hospitals with similar case mixes. Therefore we included in the measure all admissions except those for which full data was not available or for which 30-day readmission cannot reasonably be considered a signal of quality of care. Patient is alive upon discharge Rationale: Patients who die during the initial hospitalization cannot be readmitted. Patient is not transferred to another acute care hospital upon discharge Rationale: In an episode of care in which patient is transferred among hospitals, responsibility for the readmission is assigned to the final discharging hospital. Therefore these intermediate admissions within a single episode of care are not eligible for inclusion. Patient is 65 or older Rationale: Younger Medicare patients represent a distinct population with dissimilar characteristics and outcomes. Patients admitted for a condition category with high competing mortality risk in the post-discharge period are excluded. A "high competing mortality risk condition category" is one for which there were more patients who died postdischarge without being readmitted than there were patients who were readmitted. In addition the quality signal may be dwarfed by the unavoidable severity of illness. The dataset also includes data on each patient for the 12 months prior to the index admission and the 30 days following discharge. Enrollment and postdischarge mortality status were obtained from the Medicare Denominator file, which contains beneficiary demographic, benefit, coverage, and vital status information. Comorbidities were assessed using data from the index admission and any admission in past year. The Medicare outpatient (Part B) data were not included because 1) this was technically cumbersome, and 2) it would make expanding the measure later to an all-payer population very difficult (all-payer data typically includes only data for hospitalized patients). Rather than assume that effect of risk factors would be homogeneous across all discharge condition categories, we assessed the performance of a single model versus multiple models. Our analyses showed consistently that a single model did not perform as well as multiple models, independently of how we defined the multiple models. The multiple models approach showed better discrimination and predictive ability for readmission risk. The risk of readmission also varies according to the mix of conditions and procedures at a hospital (service mix). Finally, dividing the measure into several models may increase the practical utility of the measure by providing actionable information to hospitals. Conditions typically cared for by the same team of clinicians would therefore be expected to experience similar added (or reduced) levels of readmission risk. Therefore, we grouped discharge condition categories typically cared for by the same group of clinicians into six cohorts: medicine, surgery, cardiovascular, neurology, oncology and psychiatry. Organizing results by care team (service line) in this way will allow hospitals to identify areas of strength and weakness if the results of each component model are reported separately. This cohort includes admissions likely cared for by surgical or gynecologic teams. Minor procedures that would not have required a patient to be on the surgical service were not included in the list (for example: breast biopsy). Procedures that would generally accompany other, more major, procedures were also not included in the list on the assumption that patients undergoing these procedures would also undergo another procedure on the list (for example, intraoperative cholangiogram). We will consult surgeons from various specialties to confirm our list of surgical procedures.
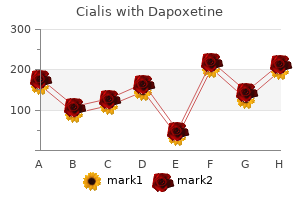
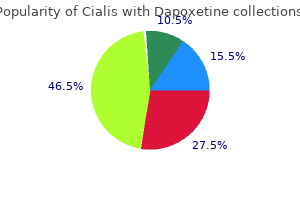
The registered mark "Cigna" and the "Tree of Life" logo are owned by Cigna Intellectual Property erectile dysfunction medication list cialis with dapoxetine 40/60 mg with mastercard, Inc erectile dysfunction effects on women generic cialis with dapoxetine 20/60mg overnight delivery. All products and services are provided by or through such operating subsidiaries and not by Cigna Corporation. Such operating subsidiaries include Connecticut General Life Insurance Company, Cigna Health and Life Insurance Company, Cigna Behavioral Health, Inc. All other medical plans in these states are insured or administered by Connecticut General Life Insurance Company or Cigna Health and Life Insurance Company. A group of admissions for patients with related condition categories or procedure categories; this measure includes seven cohorts, each with its own risk model (see Section 2. A variable in the risk-adjustment model intended to account for patient comorbid conditions or age. The variation among hospitals in the types of conditions they care for and procedures they provide. While it is helpful to assess readmission rates for specific groups of patients, these conditions account for only a small minority of total readmissions. Briefly, we developed the measure as an all-condition measure designed to capture unplanned readmissions within 30 days of discharge. The measure includes all admissions except those for which a subsequent readmission would not be considered a quality signal. The measure does not count planned readmissions in the measure outcome, since they do not represent a quality signal. The overall risk-standardized readmission rate is derived from a composite of seven statistical models built for groups of admissions that are clinically related. The seven risk adjustment models will be tested for reliability in a split sample dataset combining two calendar years (2007 and 2008), and the stability of the measure over time will be tested using data from 2009. Although we developed the measure using Medicare data, the measure will also be tested in and adapted for all-payer datasets. Some readmissions are unavoidable and result from inevitable progression of disease or worsening of chronic conditions. However, readmissions may also result from poor quality of care or inadequate transitional care. Transitional care includes effective discharge planning, transfer of information at the time of discharge, patient assessment and education, and coordination of care and monitoring in the post-discharge period. Numerous studies have found an association between quality of inpatient or transitional care and early (typically 30-day) readmission rates for a wide range of conditions. Furthermore, randomized controlled trials have shown that improvement in the following areas can directly reduce readmission rates: quality of care during the initial admission; improvement in communication with patients, their caregivers and their clinicians; patient education; predischarge assessment; and coordination of care after discharge. Widespread application of these clinical trial interventions to general practice has also been encouraging. Since 2008, 14 Medicare Quality Improvement Organizations have been funded to focus on care transitions, applying lessons learned from clinical trials. We are now soliciting comments from the general public via a public comment period. This measure reports the hospital-level, risk-standardized rate of unplanned all-cause readmission after admission for any condition within 30 days of hospital discharge. The measure comprises a single summary score, derived from the results of seven different models, one for each of the following cohorts (groups of discharge condition categories or procedure categories): general medicine, surgery/gynecology, cardiorespiratory, cardiovascular, neurology, oncology, and psychiatry, each of which will be described in greater detail below. The measure covers 95% of hospitalizations occurring in 2008 in this population, and includes 88% of readmissions following those hospitalizations. We excluded admissions for which we considered readmission not to be a signal of quality of care (patients who leave against medical advice, or have a discharge condition category with very high post-discharge mortality). To compare readmission performance across hospitals, we accounted for differences in patient characteristics (patient case mix) as well as differences in mixes of services and procedures offered by hospitals (hospital service mix). The datasets were restricted to inpatient data, and included data on each patient for the 12 months prior to the index admission and the 30 days following discharge. We collapsed these discharge condition categories into seven major cohorts according to care teams (hospital service lines) and built a separate model for each one of these cohorts. We did not risk-adjust for diagnoses that may have been a complication of care during the index admission.
Keep pressing down on the plunger while you take the needle out of the skin at the same angle as inserted (See Figure I) erectile dysfunction vacuum device generic 20/60mg cialis with dapoxetine mastercard. Put the used syringe into your puncture resistant container (See "How do I throw away used syringes If your injection is given by another person zantac causes erectile dysfunction buy generic cialis with dapoxetine on line, this person must also be careful when removing the syringe and disposing of the syringe to prevent accidental needle stick injury and passing infection. Do not throw away (dispose of) loose needles and syringes in your household trash. Do not use the Autoinjector if it appears to be damaged or if you have accidentally dropped the Autoinjector. If you are opening the box for the first time, check to make sure that it is properly sealed. Do not use the Autoinjector if the expiration date has passed because it may not be safe to use. If the expiration date has passed, safely dispose of the Autoinjector in a sharps container and get a new one. Place the Autoinjector on a clean, flat surface and let the Autoinjector warm up for 45 minutes to allow it to reach room temperature. If the Autoinjector does not reach room temperature, this could cause your injection to feel uncomfortable and it could take longer to inject. If the Autoinjector is not used within 3 minutes of the cap removal, the Autoinjector should be disposed of in the sharps container and a new Autoinjector should be used. Hold the Autoinjector comfortably in 1 hand by the upper part, so that you can see the Window area of the Autoinjector (See Figure F). To unlock it, press the Autoinjector firmly against your pinched skin until the needle-shield is completely pushed in (See Figure I). If you do not keep the needle-shield completely pushed against the skin, the green Activation button will not work. Keep the green button pressed in and continue holding the Autoinjector pressed firmly against your skin (See Figure J). If you cannot start the injection you should ask for help from a caregiver or contact your healthcare provider. Watch the purple indicator until it stops moving to be sure the full dose of medicine is injected. The needle-shield will then move out and lock into place covering the needle (See Figure L). If the Window area is not filled by the purple indicator then: o the needle-shield may not have locked. Do not touch the needle-shield of the Autoinjector, because you may stick yourself with the needle. If the needle is not covered, carefully place the Autoinjector into the sharps container to avoid any injury with the needle.
Glomerular scarring is associated with downstream tubular atrophy and interstitial fibrosis erectile dysfunction treatment muse discount cialis with dapoxetine 40/60mg line. The degree of chronic irreversible damage is most easily assessed from the amount of interstitial fibrosis and tubular atrophy erectile dysfunction insurance coverage cialis with dapoxetine 20/60 mg with visa. The assessment of chronic damage from the biopsy must always be interpreted together with the clinical data to avoid misinterpretation if the biopsy is taken (by chance) from a focal cortical scar. Clinicians should pay attention to the contents and detailed descriptions of active or chronic histopathologic features, and not just the diagnosis, in the biopsy report. Internationally validated scoring systems have been developed for some entities. Repeat kidney biopsy should be performed if the information will potentially alter the therapeutic plan or contribute to the estimation of prognosis. Occasionally, sufficient uncertainty regarding the response to management or the progression of kidney disease may be present to warrant a repeat biopsy, even in patients with a well-established diagnosis. Local cost-benefit analysis applied to the clinical decision-making for the care of individual patients may be necessary. However, 24-hour urine collection can also be subject to error due to over-collection or under-collection. Simultaneous measurement of urine creatinine and protein in an aliquot of an intended 12 to 24-hour urine collection is a good compromise that yields useful and reasonably consistent results. This effect is seen to a lesser extent when marked (nephrotic range) proteinuria is present. Simultaneous measurement of urine sodium on the 24-hour urine collection can help determine whether high sodium intake contributed to worsening proteinuria. Nephrotic range proteinuria is not always associated with "nephrotic syndrome", in that hypoalbuminemia may not be present. If a 24-hour urine collection cannot be obtained, use an alternative method to quantify proteinuria. All these methods have limitations, but are informative when sequential measurements are made in each subject. Plasma clearance of nonradioactive iohexol as a measure of glomerular filtration rate. Estimating glomerular filtration rate for the full age spectrum from serum creatinine and cystatin C. Corticosteroids Significantly Increase Serum Cystatin C Concentration without Affecting Renal Function in Symptomatic Heart Failure. Evaluation of hematuria Hematuria is one of the cardinal manifestations of glomerular disease. The initial detection of hematuria is often by "dipstick" analysis of a random urine specimen. Dipsticks are very sensitive for detection of hemoglobin in urine (free or erythrocyte-related) with very few false negatives (except in patients taking large amounts of vitamin C), but false positives in myoglobinuria or hemoglobinuria. Macroscopic or gross hematuria usually imparts a reddish or brownish "smoky" appearance to voided urine depending on urine pH. An abnormal dipstick test for blood should be confirmed by a microscopical examination of a fresh centrifuged urine sediment by phase-contrast microscopy or brightfield optics under low and high-power magnification. Staining of the urine sediment (Sterrnheimer-Malbin) can aid in the recognition of cells and formed elements. It should be noted that among the few erythrocytes seen in a normal properly collected urine, all are of a glomerular (dysmorphic) type. The prognostic implications of the persistence and magnitude of hematuria can have a very significant impact on long-term outcomes of glomerular disease. As such, findings often represent continued "low-grade" activity of the underlying glomerular inflammatory process. Periodic monitoring of the presence and magnitude of hematuria should be a part of the care process for all forms of glomerular disease, in our opinion.
Discount 40/60 mg cialis with dapoxetine amex. 5 Simple Ways To Cure Weak Erection (Erectile Dysfunction -- Causes and Treatment).