"Maxolon 10 mg low price, syarat diet gastritis".
By: X. Corwyn, M.A.S., M.D.
Co-Director, New York Institute of Technology College of Osteopathic Medicine at Arkansas State University
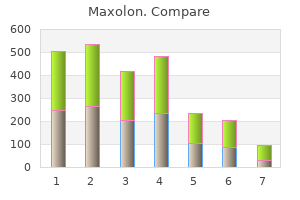
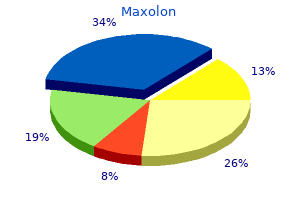
However gastritis diet x garcinia buy 10 mg maxolon, a sham-controlled gastritis diet 50\/50 order maxolon without prescription, follow-up study by the same group in 25 manic patients found no difference between active and sham treatment, despite using the same treatment approach (Kaptsan et al. In both studies, most patients were on concurrent medications (lithium, anticonvulsants, and/or antipsychotic medications). Mania scores improved by 50% or more in eight of nine and six of eight subjects in these studies. Bipolar depressed patients were included in some of the above studies, but results for these patients were mostly not presented separately, apart from reports of mood switching (see below). Patients had been withdrawn from concurrent medications which were likely to have an antidepressant effect. While other factors may have contributed to a lowered seizure threshold in this case, it is unknown whether manic patients may be more susceptible to induced seizures. Differences in their apparent speed of therapeutic action, effectiveness, and adverse effect profiles are of potential mechanistic as well as clinical significance. Expanding the definition of response to include lack of manic symptoms did not increase the response rate (Nierenberg et al. Patients undergoing lesion procedures are drawn from the extreme end of the treatment-refractory spectrum. This is important to consider when comparing outcomes across treatments, since achieving and maintaining therapeutic gains are expected to be inherently more difficult in the patient subgroups undergoing ablation. The possibility that depressive and manic symptoms respond differentially to ablation of fronto-basal-thalamic pathways is important both clinically and mechanistically. Several new developments are under way in somatic treatments for depression and it is likely that these will also be therapeutically relevant for the treatment of both bipolar depression and acute mania. Convuls Ther 4:115 125 Altshuler L, Post R, Leverich et al (1995) Antidepressant induced mania and cycle acceleration: a controversy revisited. Convuls Ther 4:81 83 Andrade C, Gangadhar B, Swaminath G et al (1988b) Predicting the outcome of endogenous depression following electroconvulsive therapy. Am J Psychiatry 136:559 562 Avery D, Winokur G (1977) the efficacy of electroconvulsive therapy and antidepressants in depression. Biol Psychiatry 12:507 523 Barekatain M, Jahangard L, Haghighi M et al (2008) Bifrontal versus bitemporal electroconvul sive therapy in severe manic patients. Acta Psychiatr Scand 41:588 596 Chen R, Classen J, Gerloff C et al (1997) Depression of motor cortex excitability by low frequency transcranial magnetic stimulation. J Neurol Neurosurg Psychiatry 75:834 839 Goldberg J, Truman C (2003) Antidepressant induced mania: an overview of current controversies. Am J Psychiatry 120:935 943 Grisaru N, Chudakov B, Yaroslavsky Y et al (1998) Transcranial magnetic stimulation in mania: a controlled study. Bipolar Disord 4(Suppl 1):91 93 Henry C, Sorbara F, Lacoste J et al (2001) Antidepressant induced mania in bipolar patients: identification of risk factors. Bipolar Disord 10:701 707 Hirschfeld R, Bowden C, Gitlin M et al (2002) Practice guidelines for the treatment of patients with bipolar disorders (revision). Psychol Med 12:615 624 Jha A, Stein G, Fenwick P (1996) Negative interaction between lithium and electroconvulsive therapy a case control study. J Affect Disord 88:255 267 Loo C, Sachdev P, Haindl W et al (2003) 15 Hz and 1 Hz transcranial magnetic stimulation have different acute effects on regional cerebral blood flow in depressed patients. Psychol Med 33:997 1006 Loo C, Schweitzer I, Pratt C (2006) Recent advances in optimising electroconvulsive therapy. Int J Neuropsychopharmacol 11:883 890 Mallet L, Polosan M, Jaafri N et al (2008) Subthalamic nucleus stimulation in severe obsessive compulsive disorder. J Affect Disord 118(1 3):55 59 Medda P, Perugi G, Zanello S et al (2010) Comparative response to electroconvulsive therapy in medication resistant bipolar I patients with depression and mixed state. Psychiatry Res 128:199 202 Sackeim H, Weiman A, Gur R et al (1982) Functional brain asymmetry in the expression of positive and negative emotions. World J Biol Psychiatry 6:121 124 Schutter D (2009) Antidepressant efficacy of high frequency transcranial magnetic stimulation over the left dorsolateral prefrontal cortex in double blind sham controlled designs: a meta analysis. Psychol Med 39:65 75 Sienaert P, Peuskens J (2007) Anticonvulsants during electroconvulsive therapy: review and recommendations. Bipolar Disord 11:418 424 Sikdar S, Kulhara P, Avasthi A et al (1994) Combined chlorpromazine and electroconvulsive therapy in mania. Br J Psychiatry 164:806 810 Small J, Kellams J, Milstein V et al (1980) Complications with electroconvulsive treatment combined with lithium. Biol Psychiatry 15:103 Small J, Klapper M, Kellams J et al (1988) Electroconvulsive treatment compared with lithium in the management of manic states.
The affected systems may be as superficial as the outer layers of the skin or as deep as the heart healing gastritis with diet order maxolon amex, central nervous system gastritis treatment home purchase maxolon 10 mg mastercard, or abdominal viscera. Although a single fungus may be more commonly associated with infection involving a single organ system. Because the management of a given infection may differ according to the etiologic agent, to guide subsequent diagnostic and therapeutic efforts, it is useful to develop a differential diagnosis that includes the most likely fungal pathogens. Because the development of a fungal infection depends on factors that often outweigh the virulence potential of the infecting organism, one must take into account numerous factors such as the immune status of the host, the opportunity for interaction between host and fungus. Fungal infections often occur in very sick patients, and it is not possible to summarize here the incredibly complex interactions that ultimately lead to the establishment of infection and disease in each organ system. Instead, this chapter provides a very broad listing of the various fungi commonly associated with specific clinical manifestations and/or infections at specific body sites (Table 59-1). This information is meant to be used in conjunction with that in Chapter 60, Table 60-1, as an aid in establishing a differential diagnosis and for selection of the most likely clinical specimens that will help establish a specific etiologic diagnosis. Other factors that may be important in determining the relative frequency with which specific fungi cause disease. Table 59-1 SummaryofFungiAssociatedwithHumanDisease SystemAffected Pathogens UpperRespiratoryInfections Oropharyngeal Sinusitis Laryngeal Esophageal Candida spp. Serious infections are being reported with an ever-increasing array of pathogens, including well-known pathogenic fungi such as Candida, Cryptococcus neoformans, Histoplasma capsulatum, and Aspergillus, as well as lesser known hyaline and dematiaceous molds (see Chapter 57, Tables 57-1 and 57-2). Modern medical mycology has become the study of mycoses caused by a variety of taxonomically diverse fungi. Opportunistic mycoses pose a significant diagnostic challenge to clinicians and mycologists alike because of the complexity of the patient population at risk and the increasing array of fungi that may infect these individuals. Successful diagnosis and treatment of mycotic infections in the compromised patient is highly dependent on a team approach involving clinicians, medical mycologists, and pathologists. This chapter provides a general description of the principles of specimen collection and processing necessary for the diagnosis of most fungal infections. An overview of direct microscopy, culture, immunologic, and molecular diagnostic testing is also provided. Specific details of these and other procedures used in the diagnosis of fungal infections may be found in several reference texts listed in the Bibliography. To provide the best treatment and clinical support, it is also important to know not only that the patient is infected with a fungus but what the fungus is. Thus diagnosis of fungal infections depends on three basic laboratory approaches: (1) microbiological, (2) immunologic, and (3) histopathologic (Box 60-1). These approaches may be supplemented by molecular and biochemical methods of organism detection and identification. Use of the newer methods for detection of fungal antigens and nucleic acids offers great promise for rapid diagnosis of fungal infections. Selection of specimens for culture and microscopic examination is based not only on information obtained from clinical examination and radiographic studies but also on consideration of the most likely fungal pathogen that may cause a specific type of infection (Table 60-1). Specimens should be collected aseptically or after proper cleaning and decontamination of the site to be sampled. An adequate amount of clinical material must be submitted promptly for culture and microscopy. Unfortunately, many specimens submitted to the laboratory are of poor quality and insufficient amount and are not appropriate to make a diagnosis. Specimens should be submitted whenever possible in a sterile leak-proof container and be accompanied by a relevant clinical history. The laboratory depends on clinical information in making decisions as to the best way to process the specimen to ensure recovery of the etiologic agent. The clinical history is also useful in interpreting the results of culture and other laboratory testing, especially when dealing with specimens from nonsterile sites such as sputum and skin. Furthermore, clinical information alerts laboratory personnel that they may be dealing with a potentially dangerous pathogen such as Coccidioides immitis/ posadasii or H.
Discount 10mg maxolon with mastercard. How To Cure Gastritis Naturally | Get Rid of Gastritis Fast.
Other less common causes should be considered when symptoms are worrisome or prolonged chronic gastritis with focal intestinal metaplasia 10 mg maxolon overnight delivery. A history of sexual activity or abuse should raise the suspicion for pharyngeal gonococcal infection gastritis menu cheap maxolon 10mg online. The degree of pharyngeal inflammation is not always consistent with the severity of the complaint. Tonsillar exudates are suggestive of streptococcus but also of mononucleosis and adenovirus. Many patients with streptococcal pharyngitis have only mild erythema without tonsillar enlargement or exudates. Viral pharyngitis is usually gradual in onset with early signs of fever, malaise, and anorexia generally preceding the sore throat. Patients can experience an abrupt onset of fatigue, malaise, fever, and headache preceding the pharyngitis. The test is not considered reliable in children younger than age 5 because of a low titer of heterophile antibody. The patient warrants emergent management for airway stabilization and treatment for potentially life-threatening conditions such as epiglottitis and retropharyngeal abscess. Although nonĀ group A streptococci have been implicated in pharyngitis, they cause a self-limiting illness, are not associated with complications, and require no treatment. Gonococcal pharyngeal infections are usually asymptomatic but can cause acute pharyngitis with fever and cervical lymphadenitis. The disease is suggested by a systemic illness and grayish membrane over the tonsils and pharyngeal walls. It should be suspected in unimmunized persons or in persons from underdeveloped countries. Culture of the organism and confirmation of its toxin are necessary to confirm the diagnosis. Herpangina is a disorder characterized by fever and discrete painful, vesicular lesions of the posterior pharynx. A variety of enteroviruses cause herpangina, including enterovirus 71, although coxsackie A viruses are implicated most often. In cases in which another family member has a positive culture finding, or in which a typical scarlatina rash is present, group A streptococcus should still be considered despite negative test results. The occurrence of conjunctivitis, rhinitis, cough, and hoarseness is more indicative of a virus than group A streptococcus. Some patients demonstrate the features of scarlet fever, including circumoral pallor, strawberry tongue, and a red, sandpaper-like scarlatina rash. These are followed by development of a maculopapular rash that begins on the forehead then spreads downward. Diagnosis is made by examination of a specimen treated with potassium hydroxide or by culture. A directed H and P examination allows for successful diagnosis and, if necessary, referral for further evaluation and treatment. Masses present since birth, or with chronic drainage or recurrent episodes of swelling, are usually congenital. Constitutional symptoms such as fever, night sweats, and weight loss may indicate a malignancy or a granulomatous process. Symptoms indicating compression of the trachea, esophagus, or recurrent laryngeal nerve should be elicited because rapid progression of the mass may be life threatening. A history of recurrent infections such as thrush, sinopulmonary infections, or cellulitis may indicate an immunodeficiency syndrome. The neck is divided into two triangles: the anterior triangle, which is bounded by the mandible, the sternocleidomastoid, and the anterior midline; and the the posterior triangle, which is bounded by the sternocleidomastoid, the distal two thirds of the clavicle, and the posterior midline. However, they rarely manifest in the newborn period and occur more commonly in children aged 2 to 10 years.
Epidemiology Paracoccidioidomycosis is endemic throughout Latin America but is more prevalent in South America than Central America (see Figure 64-2) gastritis diet įąšįč maxolon 10 mg for sale. The highest incidence is seen in Brazil gastritis diet 21 cheap maxolon, followed by Colombia, Venezuela, Ecuador, and Argentina. All patients diagnosed outside of Latin America previously had lived in Latin America. The ecology of the endemic areas includes high humidity, rich vegetation, moderate temperatures, and acid soil. These conditions are found along rivers from the Amazon jungle to small indigenous forests in Uruguay. The portal of entry is thought to be either by inhalation or traumatic inoculation (Figure 64-14), although even this is poorly understood. Although infection occurs in children (peak incidence 10 to 19 years), overt disease is uncommon in both children and adolescents. Estrogen-mediated inhibition of the mold-toyeast transition may account for the 15: 1 male/female ratio of clinical disease. Most patients with clinically apparent disease live in rural areas and have close contact with the soil. Depression of cell-mediated immunity correlates with the acute progressive form of the disease. A subacute disseminated form is seen in younger patients and immunocompromised individuals with marked lymphadenopathy, organomegaly, bone marrow involvement, and osteoarticular manifestations mimicking osteomyelitis. Adults most often present with a chronic pulmonary form of the disease marked by respiratory problems, often as the sole manifestation. The disease progresses slowly over months to years, with persistent cough, purulent sputum, chest pain, weight loss, dyspnea, and fever. Although 25% of patients exhibit only pulmonary manifestations of the disease, the infection can disseminate to extrapulmonary sites in the absence of diagnosis and treatment. The mucosal lesions are painful and ulcerated and usually confined to the mouth, lips, gums, and palate. Laboratory Diagnosis the diagnosis is established by demonstration of the characteristic yeast forms on microscopic examination of sputum, bronchoalveolar lavage fluid, scrapings or biopsy of ulcers, pus draining from lymph nodes, cerebrospinal fluid, or tissue (see Table 64-2). Isolation of the organism in culture requires confirmation by demonstration of thermal dimorphism or exoantigen testing (detection of exoantigen 1, 2, and 3). Clinical Syndromes Paracoccidioidomycosis may be subclinical or progressive with acute or chronic pulmonary forms or acute, subacute, or chronic disseminated forms of the disease. Laboratoryacquired infection has been reported in an immunocompromised individual exposed to the mycelial form in culture. Treatment Itraconazole is the treatment of choice for most forms of the disease and generally must be given for at least 6 months. More severe or refractory infections may require lipid amphotericin B therapy followed by either itraconazole or sulfonamide therapy. Relapses are common with sulfonamide therapy, and both dose and duration require adjustment based on clinical and mycologic parameters. Fluconazole has some activity against this organism, although frequent relapses have limited its use for the treatment of this disease. Clinical Syndromes Talaromycosis marneffei is manifested when a susceptible host inhales conidia of T. Patients present with fever, cough, pulmonary infiltrates, lymphadenopathy, organomegaly, anemia, leukopenia, and thrombocytopenia. Skin lesions reflect hematogenous dissemination and appear as molluscum contagiosumĀlike lesions on the face and trunk. In its mold phase in culture at 25Ā° C, it exhibits sporulating structures that are typical of the genus (see Figure 64-1). Identification is aided by the formation of a soluble red pigment that diffuses into the agar (see Table 64-3). In culture at 25Ā° C to 30Ā° C, isolation of a mold that exhibits typical Penicillium-like morphology and a diffusible red pigment is highly suggestive. Microscopic detection of elliptic fission yeasts inside phagocytes in buffy coat preparations or smears of bone marrow, ulcerative skin lesions, or lymph nodes is diagnostic (see Figure 64-15). Serologic tests that detect antigen and antibody have been developed, although no standardized commercial tests are available.