"Order propecia with a visa, hair loss blood test".
By: K. Shakyor, M.A.S., M.D.
Professor, Kaiser Permanente School of Medicine
When portal abnormalities are a manifestation of infection or neoplasm hair loss cure november 2015 buy propecia amex, there may be specific associated non-hepatic findings hair loss talk propecia 5 mg cheap, such as a hypercoagulable state, anemia, or evidence of heart failure. Portal hypertension should be suspected in any patient with ascites, splenomegaly, encephalopathy, or gastroesophageal varices. Assessment should include liver chemistry, prothrombin time, serum albumin, and complete blood cell count. It is important to remember that the presence of varices does not establish whether the lesion is intrahepatic or extrahepatic, because varices can develop with presinusoidal and postsinusoidal lesions. Once this difference exceeds 12 mm Hg, variceal hemorrhage is possible; however, the risk of hemorrhage does not correlate with the extent of elevation beyond this threshold. Mesenteric angiography may be useful to visualize portal vessels directly, either when an extrahepatic cause of portal hypertension is suspected or in anticipation of elective short surgery in which definition of the anatomy is required. Hemorrhage from gastroesophageal varices (see Chapter 123) is often the initial complication of portal hypertension. Less commonly, variceal hemorrhage occurs from other sites of portosystemic collateral vessels, including the duodenum, rectum, or sites of prior abdominal surgery. Esophageal variceal hemorrhage typically occurs as painless, large-volume hematemesis or melena with minimal abdominal pain. Signs of significant volume depletion, including orthostasis and pallor, are common. Mortality from variceal hemorrhage is more a function of underlying liver disease than severity of hemorrhage per se. A gastric variceal hemorrhage is more difficult to diagnose than an esophageal one because gastric varices are not easily distinguished from prominent rugae. A rare cause of gastric variceal hemorrhage that should not be overlooked is splenic vein thrombosis due to pancreatic or retroperitoneal disease. In this setting, localized obstruction of short gastric veins leads to hemorrhage from gastric varices in the absence of esophageal varices. Hemorrhage from portal hypertensive gastropathy, also known as congestive gastropathy, refers to bleeding in the proximal stomach from submucosal veins engorged as a result of portal hypertension. Bleeding from this lesion is clinically indistinguishable from variceal hemorrhage and responds to portal decompression. Stabilizing blood pressure is the first requirement in suspected variceal hemorrhage. Liver transplantation be avoided in the stabilized individual, because it may increase portal pressure and accelerate hemorrhage. Endotracheal intubation to protect the airway is essential in the obtunded or inebriated patient to avoid aspiration and facilitate emergent endoscopy. Hemodynamic monitoring within the intensive-care unit may require placing intra-arterial or pulmonary artery catheters. Thirty to 50 per cent of bleeding episodes in patients with varices originate from non-variceal sources, particularly Mallory-Weiss tears, esophagitis, gastritis, or peptic ulcers. Two thirds of variceal hemorrhage episodes will cease spontaneously, but rapid onset of rebleeding is significant. Thus, endoscopic hemostasis is required, either when varices are actively bleeding or when they display endoscopic evidence of recent bleeding. Two endoscopic methods are equally effective in arresting active hemorrhage in more than 95% of patients: (1) direct or paravariceal injection with 1 to 2 mL of a sclerosant (ethanolamine oleate or sodium tetradecyl) or (2) band ligation, in which a rubber ligature is placed around the varix. Band ligation is associated with a lower incidence of esophageal ulceration and more rapid variceal obliteration than sclerotherapy. Pharmacologic control of acute hemorrhage may be achieved using either a combination of intravenous vasopressin (0. Although more costly, somatostatin analogues carry less systemic hemodynamic side effects than vasopressin. In patients who continue to bleed after endoscopic or pharmacologic therapy, a Minnesota or Sengstaken-Blakemore tube can be used for balloon tamponade of vessels at the gastroesophageal junction. Only the gastric balloon should be inflated (250 mL for Sengstaken tube, 450 mL for Minnesota tube); inflating the esophageal balloon or using these devices in patients with hiatal hernias is associated with significant risk of esophageal perforation.
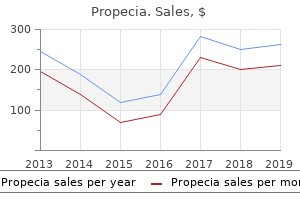
More recently hair loss in men 70s clothing generic 5mg propecia with visa, the addition of ribavirin hair loss cure propecia generic propecia 1 mg without a prescription, an oral nucleoside analogue, to alpha interferon therapy has increased the sustained response rate substantially. Thus a sustained virologic response at 6 months after treatment is highly predictive of long-term remission and resolution of disease, and it may indicate eradication of the infection. In general, the virologic features are most strongly associated with a sustained response. Thus, the combination of alpha interferon and ribavirin for 48 weeks yields overall-sustained virologic response rates of 30 to 40%. These differences are clinically important in determining the optimal regimen of treatment. Among patients with genotypes 2 and 3, the sustained response rates are 60 to 70%, and these rates are achieved by a 24-week course of therapy. In contrast, among patients with genotype 1, sustained responses are more common with a 48-week course of therapy (25 to 30%) than with a 24-week course (15 to 20%). The contraindications to alpha interferon therapy are advanced liver disease, renal failure, severe immunosuppression, solid organ transplantation, cytopenia, and active substance abuse. Ribavirin therapy is contraindicated in patients with hemolysis, anemia, significant coronary or cerebrovascular disease, or renal insufficiency. As ribavirin is teratogenic, it is essential that women practice adequate contraception during therapy and for at least 6 months thereafter. The side effects of interferon and ribavirin must be reviewed carefully before starting therapy. Thereafter, the major side effects are fatigue, malaise, depression, difficulty in concentrating, bone marrow suppression, and, in rare instances, bacterial infections or induction of autoimmune disease. Side effects of ribavirin include a dose-related hemolysis that usually results in a 5 to 15% decrease in hemoglobin level, mild itching, and nasal congestion. Even with combination therapy, the sustained response rate to interferon treatment in hepatitis C is less than 50%, and many patients find the therapy difficult to tolerate. For patients with decompensated liver disease due to hepatitis C, liver transplantation (Chapter 155) is indicated. It is characterized by presence of autoantibodies, high levels of serum immunoglobulins, and frequent association with other autoimmune diseases. The disease has been given a variety of names since it was first described in the 1950s, but in 1992 the International Autoimmune Hepatitis Group recommended the term autoimmune hepatitis and established diagnostic criteria. Two types of autoimmune hepatitis have been described: Type 1 or classic autoimmune hepatitis and Type 2 autoimmune hepatitis. Both forms are more common among women than men and have similar clinical and serum biochemical features. Type 2 autoimmune hepatitis is found largely in Europe and typically affects young women or girls. Autoimmune hepatitis is one of the three major autoimmune liver diseases, along with primary biliary cirrhosis and primary sclerosing cholangitis. Also within this group of autoimmune liver 796 diseases are variant forms of autoimmune hepatitis, which have been termed "overlap syndromes" because they share features of autoimmune hepatitis and another type of chronic liver disease, and "outlier syndromes," which have features of autoimmune hepatitis but do not to meet criteria established by the International Autoimmune Hepatitis Group. The pathogenesis of autoimmune hepatitis is not known, but it is believed to be caused by autoimmune reactions against normal hepatocytes. The disease appears to occur among genetically predisposed individuals upon exposure to as yet unidentified noxious environmental agents, thereby triggering an autoimmune process directed at liver antigens. Autoimmune hepatitis is a heterogeneous disease with a wide spectrum of clinical manifestations. Furthermore, autoimmune hepatitis is usually progressive and leads to end-stage liver disease if not treated with immunosuppression. The disease is more common in women than men and typically has its onset either in childhood and young adulthood (between the ages of 15 and 25) or around the time of menopause (between the ages of 45 and 60 years). The disease, particularly Type 2 autoimmune hepatitis, can occur in young children. In some patients it is detected before the onset of symptoms and jaundice if elevated serum aminotransferase levels are found on a routine health evaluation. Abnormalities in routine liver test results are also similar to those found in other forms of chronic hepatitis with elevations in serum aminotransferase levels. Elevations in bilirubin or alkaline phosphatase levels indicate more severe or advanced disease.
Discount propecia master card. GOLDWELL DUALSENSES 2017. RICH REPAIR.
Hepatocerebral degeneration is a chronic unremitting motor disorder of variable severity (tremor curezone hair loss purchase propecia 1 mg fast delivery, rigidity hair loss 8 week cycle order online propecia, hyperreflexia, or signs of advanced pyramidal, extrapyramidal, and cerebral dysfunction) in addition to recurrent episodes of classic overt hepatic encephalopathy. This extremely rare disorder usually occurs in patients with massive portosystemic shunts (often surgically created); it responds poorly to therapy. Spastic paralysis, which is the least common presentation of hepatic encephalopathy, occurs only rarely in patients with chronic hepatic encephalopathy and/or hepatocerebral degeneration; it also is very difficult to treat. Preclinical and mild hepatic encephalopathy (stages 0-1, 1, 2) can be recognized by poor performance on psychometric tests. Clinically suspected hepatic encephalopathy may be objectively confirmed by prolonged reaction time to visual or auditory evoked potentials. Measurement of serum ammonia level is non-sensitive because hepatic encephalopathy can occur in patients with a normal blood ammonia level. Advanced hepatic encephalopathy (stages 3-4) is not difficult to recognize clinically. Consistent with the current theories about the pathogenesis of hepatic encephalopathy, there are four general targets/goals of therapy: (1) intestines: decrease production and absorption of possible toxins; (2) liver: improve liver function and clearance of toxins; (3) blood-brain barrier: prevent penetration of potential toxins into the brain; and (4) brain: correct abnormal neuronal activity. The small and large intestines are the main sources of ammonia and the other toxins that may cause hepatic encephalopathy. Lactulose is a non-absorbable disaccharide; by causing acidification of intestinal contents and acting as a cathartic agent, it decreases the absorption of ammonia into the blood stream. Lactulose can be given orally, through a nasogastric tube, or rectally (less effective) in doses of 30 to 120 mL/day to produce two to four soft bowel movements per day. Some patients are not able to tolerate lactulose because of frequent side effects of flatulence, abdominal cramps, and its excessively sweet taste. Poorly absorbed antibiotics, such as neomycin (initially 1-2 g orally four times a day), alter intestinal flora and thus decrease the production of nitrogenous substances by bacteria and reduce the release of ammonia into the blood. Because chronic neomycin can promote colonization with resistant organisms and may be absorbed systemically and cause nephrotoxicity and ototoxicity, neomycin should be used for short periods of time, and the dose should be decreased to 1 to 2 g/day after achievement of the desired clinical effect. Alternatively, metronidazole can be given at 250 mg orally three times a day alone or with neomycin; the most common side effects of chronic metronidazole are peripheral neuropathy and dysgeusia. Dietary restriction of protein can decrease the production of ammonia by colonic bacteria. However, long-term dietary protein restriction can lead to malnutrition and can be harmful, especially in patients with decreased liver synthetic function. If tolerated, a positive nitrogen balance may improve hepatic encephalopathy by promoting hepatic regeneration and increasing the capacity of muscle to detoxify ammonia. Clinical trials are currently evaluating the role of supplementary zinc, which is a cofactor of urea cycle enzymes, and ornithine-aspartate, which can reduce blood ammonia by stimulating ureagenesis and synthesis of glutamine in the liver. Benzoate, which conjugates with glycine to form hippuric acid, and phenylacetate, which conjugates with glutamine to form phenylacetylglutamine, can provide potential alternative pathways for the urinary excretion of nitrogen-containing molecules. Branched-chain amino acids (valine, leucine, isoleucine) given orally or parenterally can theoretically normalize the aromatic amino acid/branched-chain amino acid ratio and prevent excessive penetration of aromatic amino acids into the brain. However, clinical trials have failed to show major beneficial effects of branched-chain amino acid administration, and this treatment is not generally recommended. Flumazenil may transiently improve the mental state in selected patients with hepatic encephalopathy. However, this drug is available only for intravenous injection and is not useful for the chronic therapy. Bromocriptine does not improve the level of consciousness in patients with hepatic encephalopathy, but it may be useful for treatment of extrapyramidal manifestations in selected patients with hepatocerebral degeneration or spastic paralysis. Prevention of clinically overt hepatic encephalopathy includes early identification and timely correction of reversible precipitating factors, strict adherence to the diet, prevention of constipation, improvement of liver function, and supportive therapy. Acute liver failure is a clinical syndrome caused by sudden, massive destruction of liver cells or by insults that severely inhibit the ability of hepatocytes to accomplish their normal functions. The duration of time that elapses between the clinical recognition of liver disease and the onset of hepatic encephalopathy (and/or impairment of liver functions) has been used to classify acute liver failure: within 2 weeks-fulminant liver failure; within 2 to 8 weeks-subfulminant liver failure; and within 8 to 24 weeks-late onset liver failure. Patients with a shorter interval from the onset of jaundice to the development of hepatic encephalopathy generally have a better prognosis, with a lower incidence of ascites but a greater incidence of cerebral edema compared with those who develop hepatic encephalopathy more slowly. Acetaminophen ingestion is responsible for 10% of acute liver failure cases in the United States. Massive liver cell necrosis from other drugs such as isoniazid, halogenated anesthetics, phenytoin, propylthiouracil, and sulfonamides accounts for another 10%; acute liver failure can also be induced by drug interactions, as seen with alcohol and acetaminophen, acetaminophen and isoniazid, and isoniazid and rifampin.
Surgical resection in the remaining patients can achieve a 5-year survival rate of 37 to 44% hair loss 9gag purchase 5mg propecia with amex. Palliation is generally achieved by percutaneous or endoscopic placement of stents to ensure passage of bile hair loss in men 50s costume buy generic propecia 5 mg online, with surgical drainage used in selected patients. Adjuvant therapy for cholangiocarcinoma has included radiation therapy (external-beam radiation or endoluminal brachytherapy) and chemotherapy with 5-fluorouracil, doxorubicin, and mitomycin-C; response rates for these modalities are approximately 20%. It has been associated with exposure to vinyl chloride, Thorotrast, and arsenic compounds. The tumor usually presents as abdominal pain and a palpable right upper quadrant mass, but progressive liver failure and acute hemoperitoneum have been described. Angiography shows a characteristic blush and persistence of peripheral enhancement with a central hypovascular area. Treatment consists of surgical resection, which is difficult to achieve owing to the advanced stage of the tumor at the time of diagnosis. Other rare hepatic tumors in the adult liver include squamous cell carcinoma (usually arising in congenital cysts), embryonal sarcoma, fibrosarcoma, leiomyosarcoma, liposarcoma, biliary cystadenocarcinoma, mucoepidermoid carcinoma, malignant rhabdoid tumor, and carcinosarcomas. These tumors cause symptoms and signs similar to the more common hepatic malignant neoplasms. Diagnosis is usually made by needle biopsy during evaluation or at the time of resection. Metastatic tumors are the most common malignant neoplasms of the liver in the United States. The most frequent primary tumors to metastasize to the liver include those originating in the gastrointestinal tract (colon, stomach, pancreas, esophagus, extrahepatic cholangiocarcinoma), lung, and breast. Other solid tumors that metastasize to the liver include neuroendocrine tumors, bladder cancer, melanoma, and renal cell carcinoma. The liver is also an extranodal site of involvement for lymphomas and malignant histiocytosis. Metastatic tumors usually present in the setting of known extrahepatic malignancy, and the diagnosis is often suspected before a liver lesion is found. Metastatic tumors may occasionally present as diffuse involvement and cause rapidly progressive hepatic dysfunction and diagnostic uncertainty. Prognosis is poor once tumor metastases have been found, with a mean survival after diagnosis of 6 months. Selected patients may be surgical candidates for resection of isolated metastases, particularly those from colorectal adenocarcinoma. Patients who have unresectable disease may be offered systemic chemotherapy with the specific protocol depending on the origin of the primary tumor. Provides a comprehensive and thorough review of screening strategies for the early detection of hepatocellular carcinoma. Provides a useful approach to the evaluation of hepatic tumors with emphasis on radiological techniques currently employed. Its exocrine secretion, bile, provides detergents (bile salts) needed for digestion and absorption of lipids, as well as bicarbonate to neutralize gastric acid. Secretion of bile also has an excretory function because it serves as the major pathway for elimination of many waste products of metabolism as well as exogenous toxins. Bile is formed in bile canaliculi, a network of tubular structures within the hepatocyte plates. The walls of a canaliculus consist of specialized regions of the plasma membranes of two adjacent hepatocytes. The canalicular (biliary) domain of the hepatocyte plasma membrane is separated from the sinusoidal (plasma) domain by tight junctions that allow free passage of water but restrict movement of macromolecules. Bile salts are the most abundant organic solute of hepatic bile (bile salts are the ionized species of bile acids, and these terms are often used interchangeably by the physiologist). Bile also contains large amounts of two lipids: phosphatidylcholine (also termed lecithin) and unesterified (free) cholesterol. Bilirubin is secreted into bile as monoglucuronides and diglucuronides and is responsible for its yellow color. The total protein content of bile is low (about 1/50 of the plasma protein concentration).